| A is for Airway |
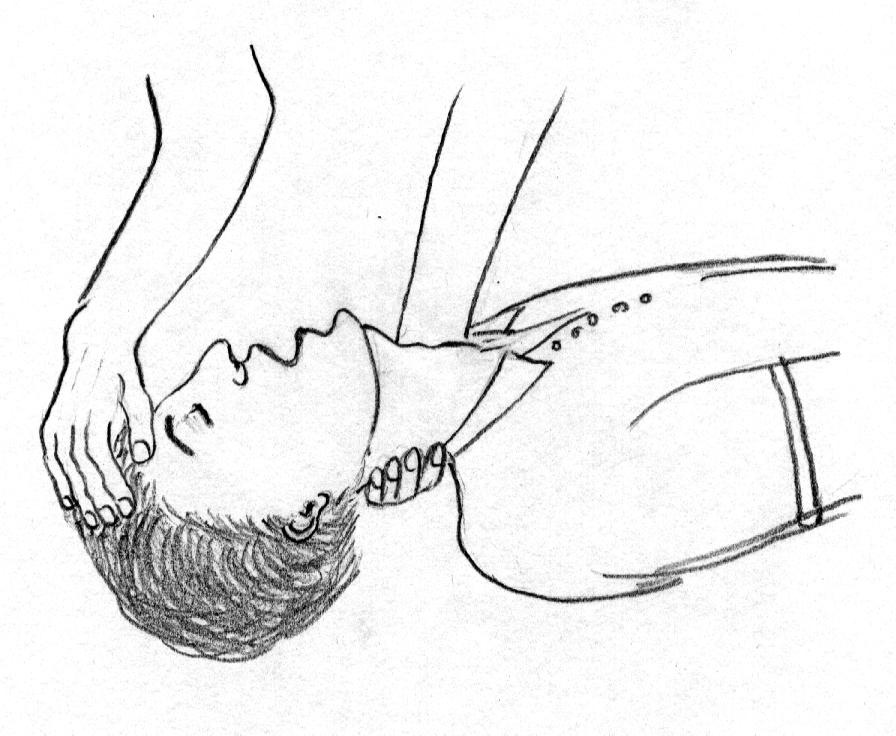
This means positioning the patient's head so that it is hyperextended, by tilting the head and lifting the chin Causes why the airway could be blocked:1) the lax tongue falls back
TRIPLE MANOUVRE
A combination of the above two methods known as Triple maneuver MODIFIED JAW THRUST METHOD Support the maxillae between the palms with elbows resting on the table
All maneuvers elevate the mandible and as the tongue is attached to the lower jaw, it is lifted up thus opening the airway. Visible material can be removed by using your fingers to scoop it out or wipe it away. Look, Listen, Feel
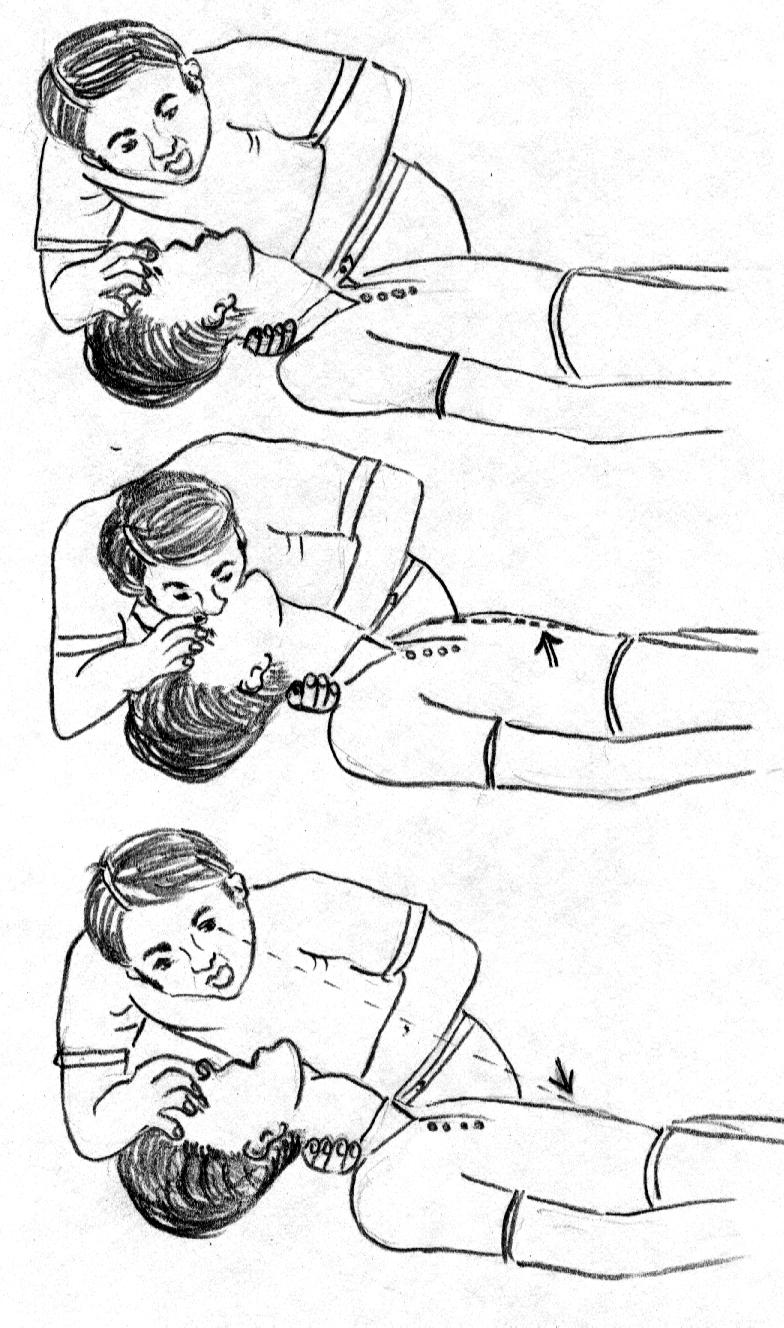
Notice how the rescuer is kneeling at a level that is next to the patient's upper arm. This position is useful when (or if) it becomes necessary to administer chest compressions. Further notice that the rescuer's ear is right above the patient's nose and mouth, and that the rescuer has turned her head so that she is looking at the patient's chest. Hence the description, "Look, listen and feel." Look at the chest to determine if it is moving. Listen for the sound of air moving in and/or out of the nose and mouth. Feel for the movement of air from the nose and/or mouth. A person who is unconscious may take infrequent gasps of air, but this is not breathing. In case of no evidence of breathing rescue breaths are initiated. In case there is no rise or fall of chest and resistance is encountered in the breaths then probably airway is blocked and must be cleared before proceeding to the next step of breaths. |
B is for Breathing |
Methods for delivering rescue breaths – Mouth to mouth Seal the nose by pinching the nostrils so air can't escape while you blow air in through the mouth. Take a breath, open your mouth and place it over the person's slightly opened mouth. Take care not to lose head tilt. Maintain a good seal around the patients mouth Now blow to inflate the person's lungs and look with the corner of your eyes for the chest rise.
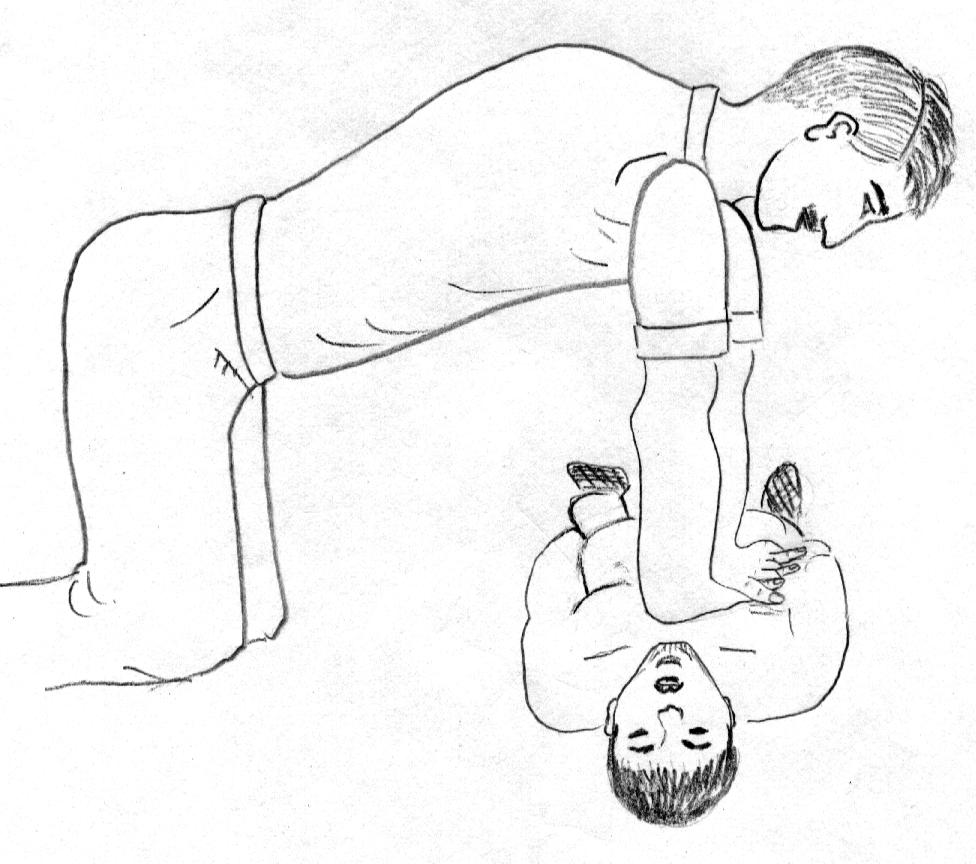
Each time rescue breaths are given ensure – the airway is opened Mouth-to-Nose is used where the casualty has sustained facial injuries that preclude using the mouth. This is indicated in cases of vomiting, bleeding injuries to the mouth and poisoning. The rescuer closes the casualty’s mouth, covers the nose with their mouth, breathes gently, then releases the casualty’s jaw to allow exhalation. Mouth-to-Nose-&-Mouth is the preferred method when resuscitating a child, as the rescuer’s mouth can cover and seal the child’s nose and mouth. Mouth-to- Stoma is used for resuscitating a casualty who breathes through a stoma, an opening in the neck, through which the casualty normally breathes. The rescuer breathes through the stoma directly into the airway while blocking the nose and mouth. Mouth-to-Mask is the most desirable method for rescue breaths as it lessens the risk of cross-infection and is more acceptable to many people than mouth-to-mouth. Masks come in various forms but they are used similarly. The mask is fitted firmly over the casualty’s nose and mouth and the rescuer delivers rescue breaths via the valve or tube thus avoiding direct contact with the casualty’s mouth or expired air. |
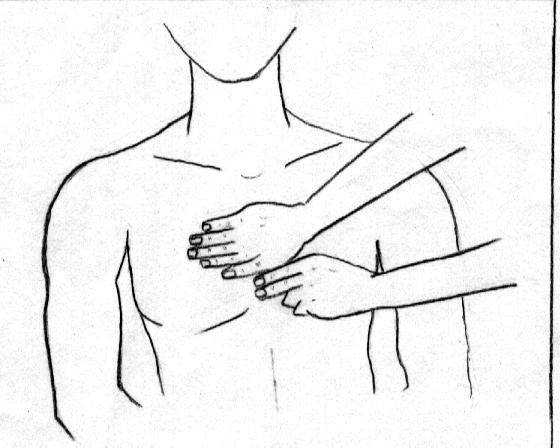
| C is for Circulation |
Check the CAROTID Pulse
After giving 2 quick breaths you need to check for a pulse. Place two fingers gently on the thyroid cartilage, then slide them off to the curve between the sternocleidomastoid and the Adam's Apple. Feel with the flat portion of the fingers, not the tips. Don't push too hard and only feel one side of the neck, for about 10 seconds. If there is a pulse: If there is no pulse: Start chest compressions Locate the correct compression point:
|