For Children over 8 years, one can generally apply the adult CPR guidelines. Cardiac arrest in the pediatric age group is rarely of cardiac origin, and more commonly results from a low oxygen level secondary to respiratory difficulty in the arrest. CPR in children has had poor outcome according to statistics as it is basically due to long periods of hypoxemia. The outcome of resuscitation from respiratory arrest before the development of a cardiac arrest is however better and hence educational programs should emphasize on prevention, early recognition of child in distress and rapid intervention before a cardiac arrest occurs. |
Indications for resuscitation in children |
Most common indications for CPR in children are:
|
Airway, Breathing and Circulation maintenance |
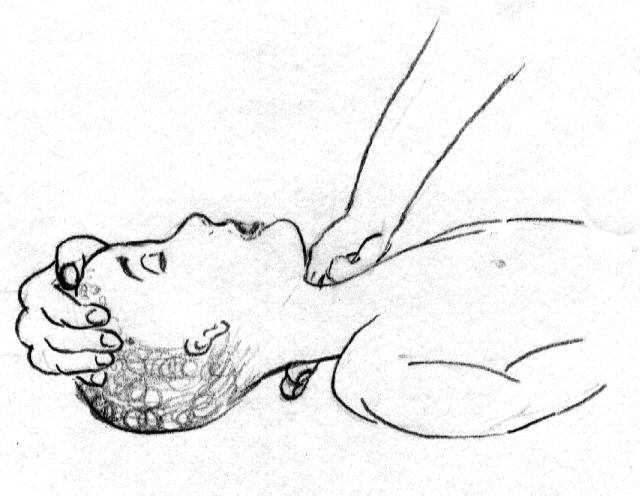
Airway: The head is not tilted too far back, only straightened out, as hyperextension or hypo extension could still obstruct the airway. Steps include a head tilt neck lift by using two fingers placed under the neck.
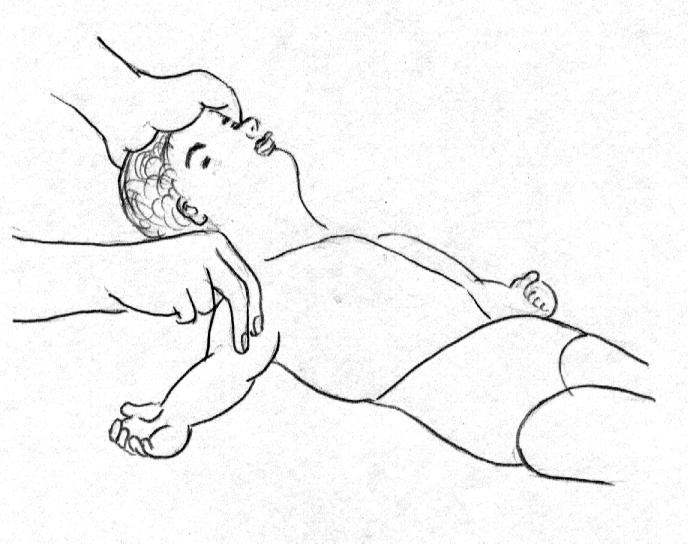
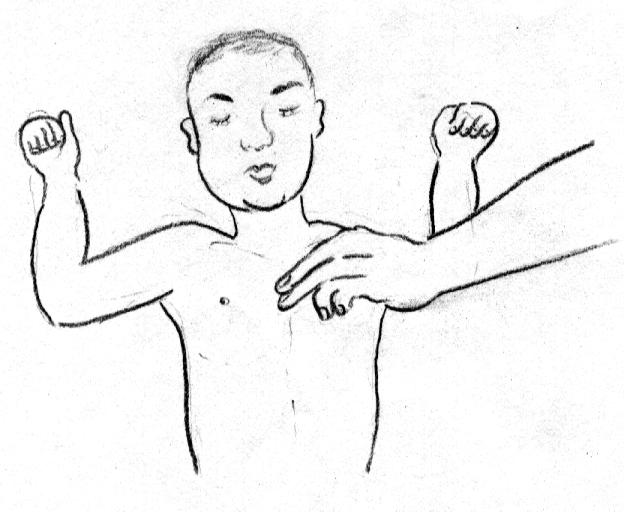
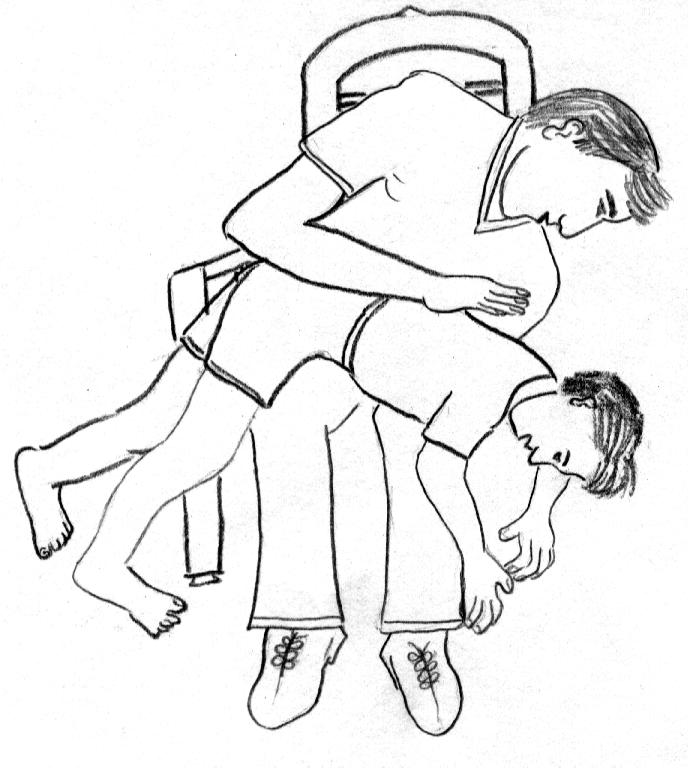
Circulation:For children over one year feel for the carotid pulse as in the case of Adult CPR. In infants the brachial or femoral arteries (refer above picture) are preferred. The artery can be felt in the cubital fossa medial to the tendon of the biceps or in the arm. Femoral artery is felt in the mid inguinal point. If pulses are not felt or pulse less than 60 per minute proceed to external chest compressions. External chest compressions:
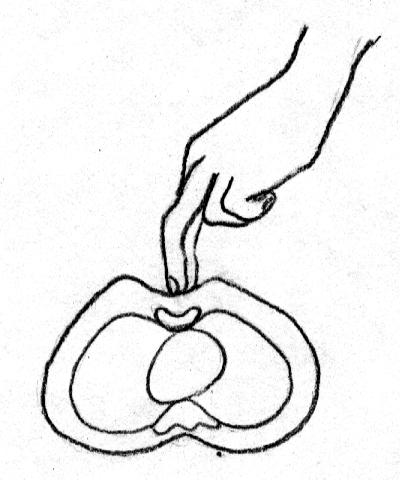
Position the child: place index finger in the chest in a line joining the child’s nipples. |
CHOKING CHILD |
Conscious children should be encouraged to cough if possible. Check the open mouth for foreign bodies and remove it. Blind finger sweeps and finger probing should be avoided. |